In independent pain practices, write-offs rarely result from a single large mistake. They accumulate quietly, one denied claim at a time, often handled at the end of a long clinic day when there is little room to revisit what already feels settled.
Most of these decisions are not careless. They are practical. Teams move on because the work is done, the patient has been seen, and there are always more claims waiting.
Over time, those routine write-offs add up to meaningful revenue loss.
What many practices eventually realize is this: the biggest revenue leak is not denials. It is how quickly denials turn into permanent write-offs.
Why write-offs deserve a second look
Most interventional pain practices will say, “Denials are killing us.”
What often hurts more is what happens next.
After reviewing multiple independent pain groups, one pattern keeps repeating. Too many dollars are being written off by habit, not by rule.
Once a claim reaches the write-off stage, it is frequently treated as a final step rather than a decision point. Denial turns into adjustment without a real pause to ask whether the claim was truly unrecoverable.
That led us to start asking one uncomfortable question during account reviews, every single time:
Is this a true write-off, or did we give up too early?
That question is what quick audits are designed to answer.
What a quick audit is and what it is not
A quick audit is not about recreating months of billing activity or reconciling totals.
It is a short, focused review designed to surface patterns, not numbers.
The goal is not to calculate revenue loss.
The goal is to identify one or two upstream issues that are causing the same denials and write-offs to repeat.
When used consistently, quick audits take minutes, not hours.
A simple four-step quick audit framework
Quick audits work best when they follow a repeatable structure that fits into existing billing workflows.
1. Pull a small, meaningful sample
Start small. Ask your team for the last 30 write-offs above an amount that actually matters in your practice.
You do not need a full report. At a minimum, you only need four data points:
- Date
- Amount
- Payer
- Reason
If pulling this takes more than a few minutes, that alone is a useful signal.
2. Force a clear reason for each write-off
Before any adjustment is approved, every write-off should be forced into one clear category:
- Forced or contractual, where the adjustment is contractually required
- Denial-driven, where the write-off follows a payer denial
- Process-driven, where something internal broke
Most practices never slow down enough to do this. That is where revenue quietly slips away.
Not all write-offs are equal, and treating them the same is where compounding loss begins.
3. Identify claims that should never be auto-written off
Some write-offs should always trigger a pause.
In particular, any write-off tied to:
- Modifier usage
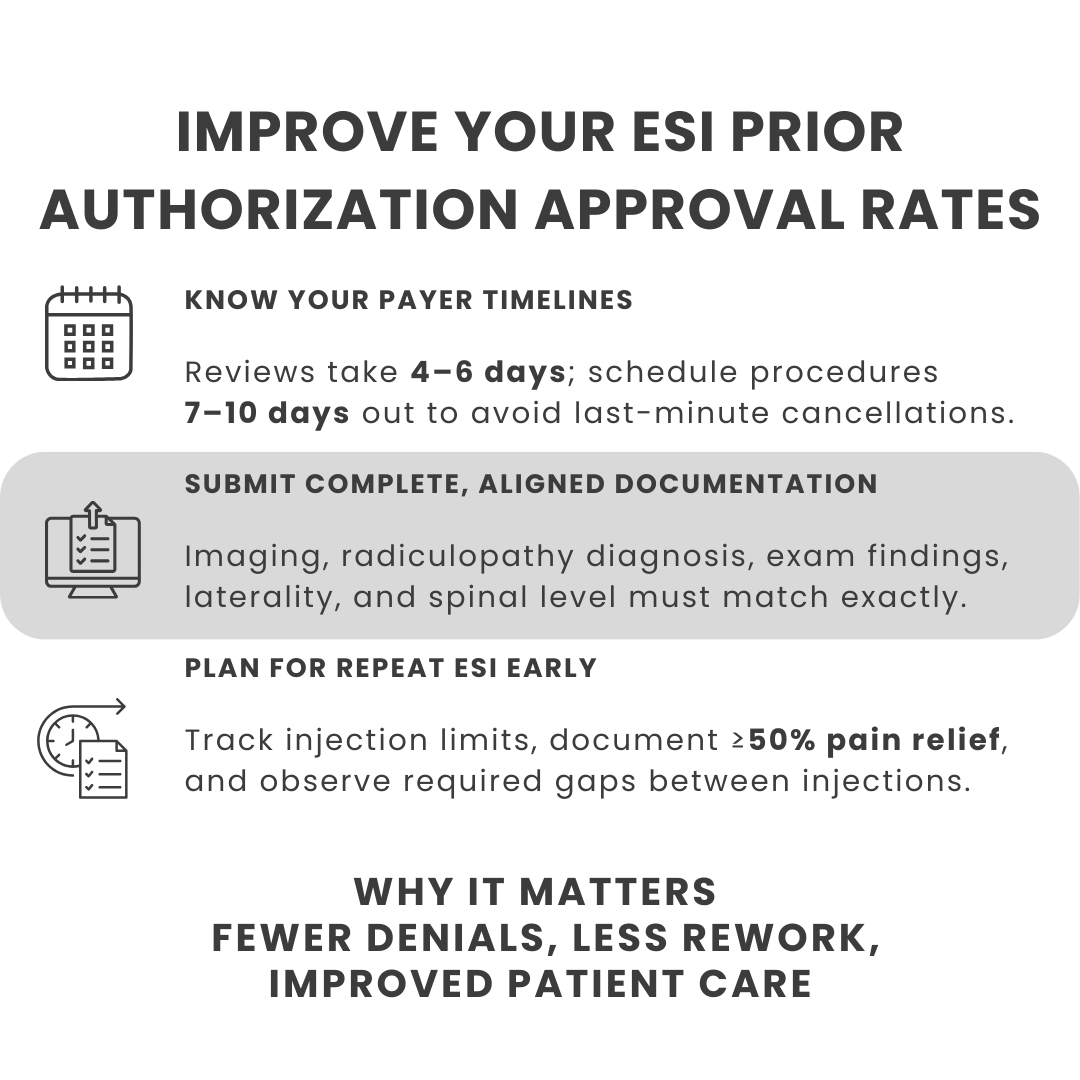
- Prior authorization
- Medical necessity documentation
- Timely filing
should never be treated as a routine adjustment.
These are not “just write-offs.” They are signals that workflows, ownership, or documentation failed upstream. Over time, these claims tend to be written off for convenience rather than lack of merit, even though many are recoverable.
Separating this group helps teams focus effort where it has the greatest return.
4. Look for patterns, not dollar totals
The value of a quick audit is not in calculating how much was lost.
It is in identifying what keeps showing up again and again.
In your next billing huddle, ask just two questions:
- What percentage of our write-offs are process-driven?
- Of those, how many involve modifiers, authorization, medical necessity, or timely filing?
| A practical takeaway for billing teams To make this process easier to run consistently, we have created a Quick Audit cheat sheet that billing teams can use during routine write-off review. 👉 Download the cheat sheet to help your team identify preventable write-offs and recurring patterns, without adding extra work. |
When the same payer, procedure, or modifier keeps appearing, that is usually not bad luck. It is a fix waiting to be designed.
What billing teams typically find
The results of quick audits are rarely surprising, but they are often clarifying.
Common findings include:
- The same documentation issue appearing across multiple claims
- Appeals submitted once, without strengthened support
- Write-offs tied to a specific workflow gap or handoff failure
- Claims abandoned even though payer policy supported appeal
Many teams discover that the default loop looks like this:
Denial → one appeal → “we tried” → adjustment.
Practices that retain more revenue treat appeals as a process, not a one-time attempt. Their appeals are anchored to specific payer or LCD language, clear diagnosis-procedure linkage, and structured arguments rather than free-text explanations.
Why quick audits matter for independent practices
Independent practices operate with lean teams and limited room for rework.
Quick audits are effective because they:
- Fit into real-world billing operations
- Create shared visibility into why money disappears
- Surface fixes that prevent repeat losses
When this discipline is applied consistently, independent pain practices often see tangible results within 60 to 90 days, including:
- 30–50% reduction in avoidable write-offs, particularly those tied to modifiers, authorization, and documentation gaps
- Real recovery on denial-driven claims, rather than automatic adjustments after a single appeal
- Cleaner accounts receivable, with fewer claims lingering or being written off prematurely
- Greater confidence across billing teams that a denial is a starting point for action, not a final outcome
| Looking for clarity? If write-offs are recurring and it is unclear which ones were truly unavoidable, a brief, focused review can help bring structure to the process. Connect with our team to discuss what you are seeing and whether a targeted review would be useful. Call us at (512) 868-1762 |
This approach does not require more staff or longer hours. It requires treating write-offs as a decision that deserves scrutiny.
Most revenue leakage in interventional pain does not start with payer policy.
It starts inside the practice, with premature surrender on recoverable claims.
Quick audits are not about assigning blame. They are about slowing the process just enough to make better decisions before write-offs become permanent.
For independent pain practices, protecting revenue often begins with one simple shift: treating write-offs as a decision, not an endpoint.