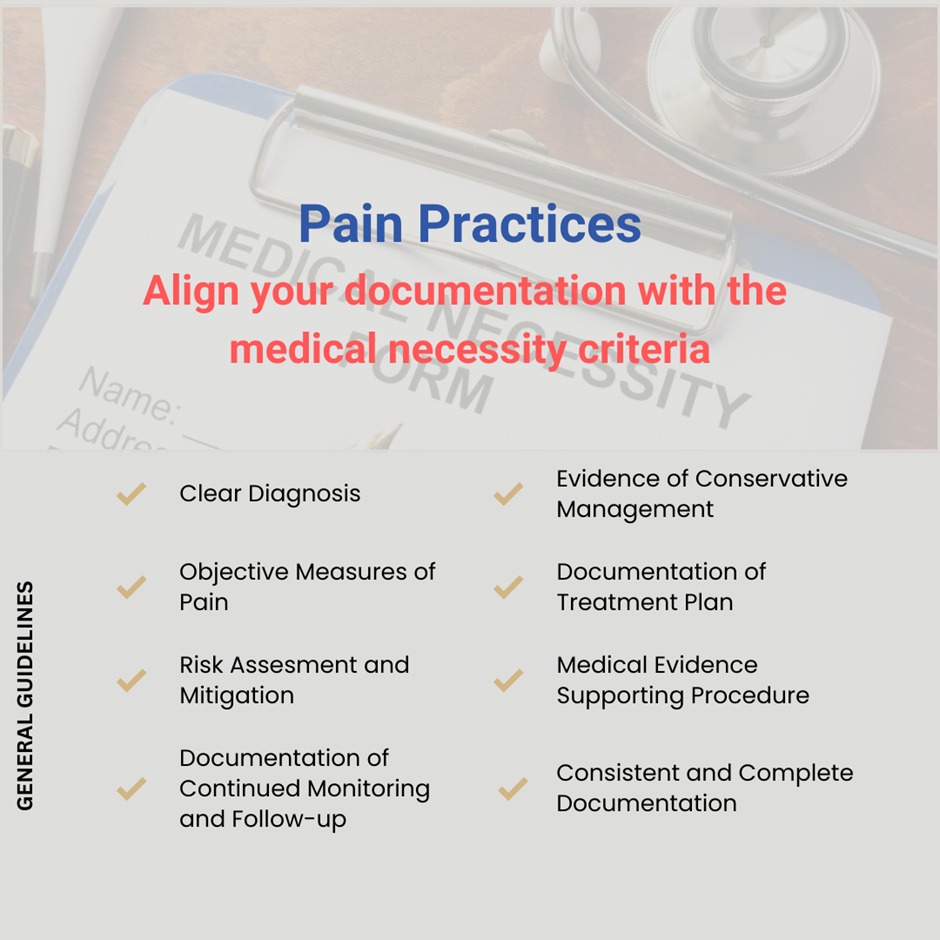
In the realm of pain management, ensuring documentation aligns with the criteria for medical necessity is paramount not only for reimbursement but also for Prior Authorization approvals.
While guidelines may vary somewhat between payers, there are overarching principles that physicians must adhere to. Here are some key points:
🔸Clear Diagnosis: Documentation should include a clear and specific diagnosis of the patient’s condition and any relevant medical history. This helps establish the medical necessity of the treatment or procedure being recommended.
🔸Evidence of Conservative Management: Insurance companies typically expect to see evidence that conservative treatments have been attempted and found ineffective before more invasive interventions are pursued. This might include medications, physical therapy, or other non-invasive therapies.
🔸Objective Measures of Pain: Physicians should provide objective measures of the patient’s pain levels, such as pain scales or descriptions of functional limitations, to demonstrate the severity and impact of the condition on the patient’s quality of life.
🔸Documentation of Treatment Plan: The physician should outline a clear treatment plan tailored to the patient’s needs and include the rationale for any recommended procedures or treatments.
🔸Risk Assessment and Mitigation: Physicians should assess and document the patient’s risk factors for potential complications or adverse outcomes associated with the proposed treatment, and any measures taken to mitigate these risks.
🔸Medical Evidence Supporting Procedure: Insurance companies may require medical evidence supporting the effectiveness and appropriateness of the proposed procedure or treatment, such as clinical guidelines, peer-reviewed studies, or expert consensus.
🔸Documentation of Continued Monitoring and Follow-up: Physicians should document plans for ongoing monitoring of the patient’s progress and arrangements for follow-up care to ensure the effectiveness and safety of the treatment over time.
🔸Consistent and Complete Documentation: All documentation should be consistent, legible, and complete, providing a comprehensive overview of the patient’s condition, treatment history, and response to interventions.
By adhering to these guidelines and ensuring thorough documentation, physicians can increase the likelihood of insurance approval for medically necessary procedures and treatments in the field of pain management.