Are you confident your team is submitting Epidural Steroid Injection (ESI) prior-authorization requests correctly, or are avoidable denials slowing your workflow and impacting revenue?
This article is the second instalment in our educational video series, created to deliver short, practical insights that help pain practices improve prior-authorization accuracy, reduce denial risk, and streamline revenue cycle operations.
In this instalment, we focus on epidural steroid injections: a high-volume procedure where prior authorization and claims issues continue to be a major operational bottleneck.
Why ESI Prior Authorization Continues to Be a Bottleneck
Epidural steroid injections are among the most performed procedures in pain management.
Despite their frequency, prior authorizations and claims for ESIs fail 25–30% of the time on the first attempt.
In most cases, denials aren’t caused by lack of medical necessity.
They stem from missed or outdated imaging, insufficient documentation of conservative therapy, unclear radicular findings, or simple mismatches between the clinical story and what payers expect to see.
| Need Help with ESI Prior Authorizations? If ESI prior auths or claims are slowing your clinic down, our team can help. We work alongside pain practices to tighten documentation, stay aligned with payer guidelines, and reduce rework from avoidable denials. Call us at (512) 868-1762 |
These gaps lead to rework, delayed care, frustrated staff, and unnecessary revenue leakage—especially when ESIs are being performed at scale.
Three High-Impact Tips to Improve ESI Prior Authorization Approval Rates
Below are three practical steps discussed in Episode 2 that can make the ESI prior authorization process significantly simpler and more predictable.
Step 1: Understand Payer Timelines and Policy Nuances
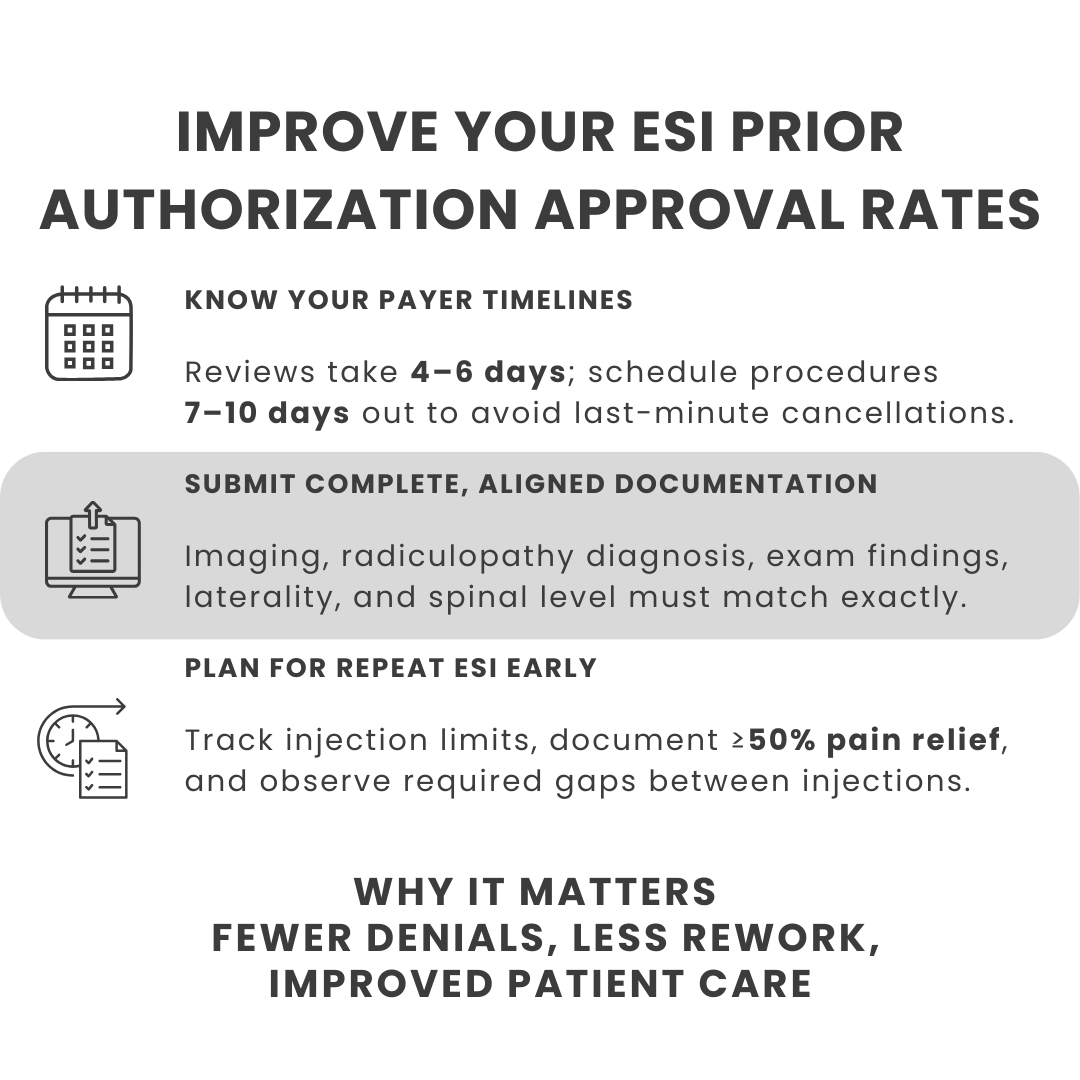
Most payers take four to six days to approve an ESI prior authorization request. To account for delays and avoid last-minute scheduling changes, it’s best to schedule patients seven to ten days out from the submission date.
It’s equally important to understand payer-specific guidelines and policy nuances. Many insurers, for example, require imaging to be no more than 24 months old at the time of the procedure. Submitting outdated imaging—even if clinically relevant—can result in automatic denial.
Aligning scheduling and documentation with these timelines helps reduce cancellations and improves both staff and patient experience.
Step 2: Confirm All Required Documentation Before Submission
Before initiating an ESI prior authorization, ensure all documentation requirements are fully met. This includes:
- Before initiating an ESI prior authorization, ensure all documentation requirements are fully met. This includes:
- A correct diagnosis of radiculopathy
- MRI or CT imaging evidence, such as disc herniation or spinal stenosis, that correlates directly with radicular symptoms
- A clinical exam documenting radiculopathy
- Clear documentation of failed conservative therapy
- Most importantly, confirmation that laterality, spinal level, and severity align precisely between the clinical notes and imaging findings
- Even minor inconsistencies between these elements can lead to denials or requests for additional information.
Step 3: Plan for Repeat ESI Procedures
Planning for repeat procedures is a critical but often overlooked part of ESI prior authorization.
Most insurers:
- Limit ESIs to three injections within a rolling 12-month period
- Require at least 50% documented pain improvement to approve subsequent injections
- Mandate a minimum three-month gap between repeat injections
Without careful tracking and documentation, repeat ESI requests are highly susceptible to denial. Building these rules into your workflow upfront helps ensure continuity of care and smoother authorization cycles.

| 👉 Help your team submit cleaner ESI authorizations the first time with our clinic-ready checklist ⬇️Download the Epidural Steroid Injection (ESI) Prior Authorization Submission Checklist |
Why Optimizing ESI Prior Authorization Matters
When ESI prior authorization workflows are poorly managed, practices face:
- Delays in patient care
- Increased administrative burden on clinical and billing teams
- Higher denial and rework rates
- Disruptions to revenue consistency
ESIs may be routine, but payer scrutiny is not. Optimizing the authorization process is essential to keeping high-volume procedures running efficiently.
| 🎥Watch the Video Here |
The ESI prior authorization process comes with its own payer-specific nuances and documentation expectations. The guidance shared in this episode is intended to help practices create consistency, reduce preventable denials, and improve operational efficiency.
As this educational series continues, we’ll keep sharing real-world, practical insights to help pain practices stay ahead of evolving authorization requirements and protect both clinical and financial outcomes.