Are you confident your team is submitting Spinal Cord Stimulation (SCS) prior-authorization requests in the most effective way, or are you playing a risky game of chance with payers?
Welcome to the very first instalment of our knowledge articles designed to deliver short, practical insights to help your practice sharpen prior-authorization accuracy, avoid common billing and denial-prevention pitfalls, and safeguard revenue.
In this debut piece, we dive into SCS prior-authorization workflows, one of the trickiest areas for approvals and share three high-impact tips that can dramatically improve your chances of approval from day one.
Why SCS Prior Authorization Requires High-Accuracy Documentation
SCS therapy, often used to manage chronic pain when conventional methods fail, is increasingly common. But with its growing use comes increasing scrutiny from payers. In fact, recent reports suggest that SCS approvals have become a “50/50 gamble,” with first-pass denial rates approaching 50%.
This high denial rate isn’t necessarily due to lack of clinical merit. It’s often the result of shifting payer coverage criteria, varying interpretations, and tight SCS documentation requirements. Many practices end up re-submitting requests multiple times, navigating exhausting peer-to-peer reviews, and managing frustrated patients and overwhelmed staff.
Meanwhile, administrative burden continues to rise. According to the American Medical Association, physicians now complete nearly 40 prior authorizations per week, diverting clinical teams from patient care. This is exactly why SCS prior authorization workflows require structure, clarity, and precision, not guesswork.
Get in Touch with Our Team for SCS Prior Authorization Support
Our experts help practices streamline SCS documentation, improve approval rates, and reduce denials across high-scrutiny procedures. Call us at (512) 868-1762
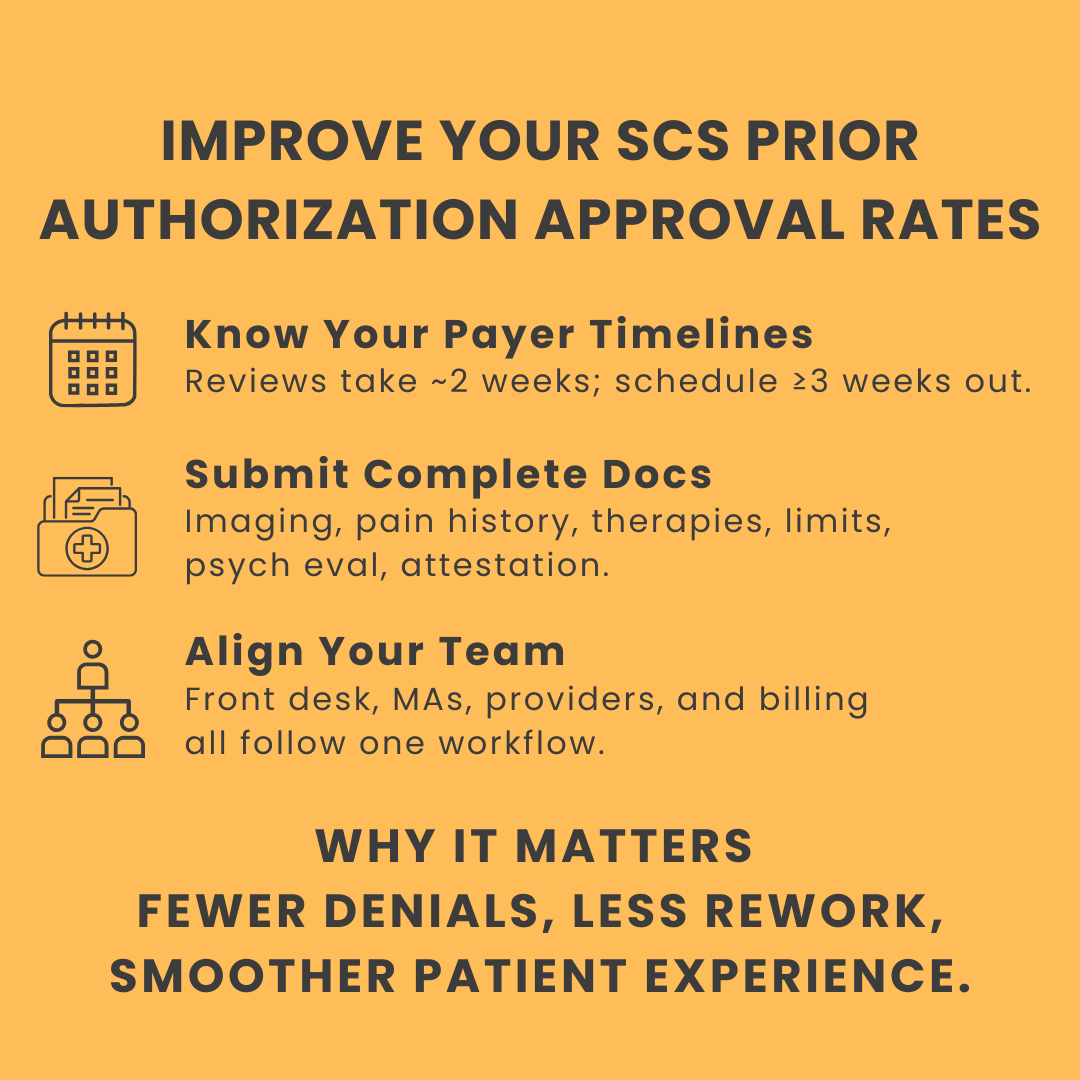
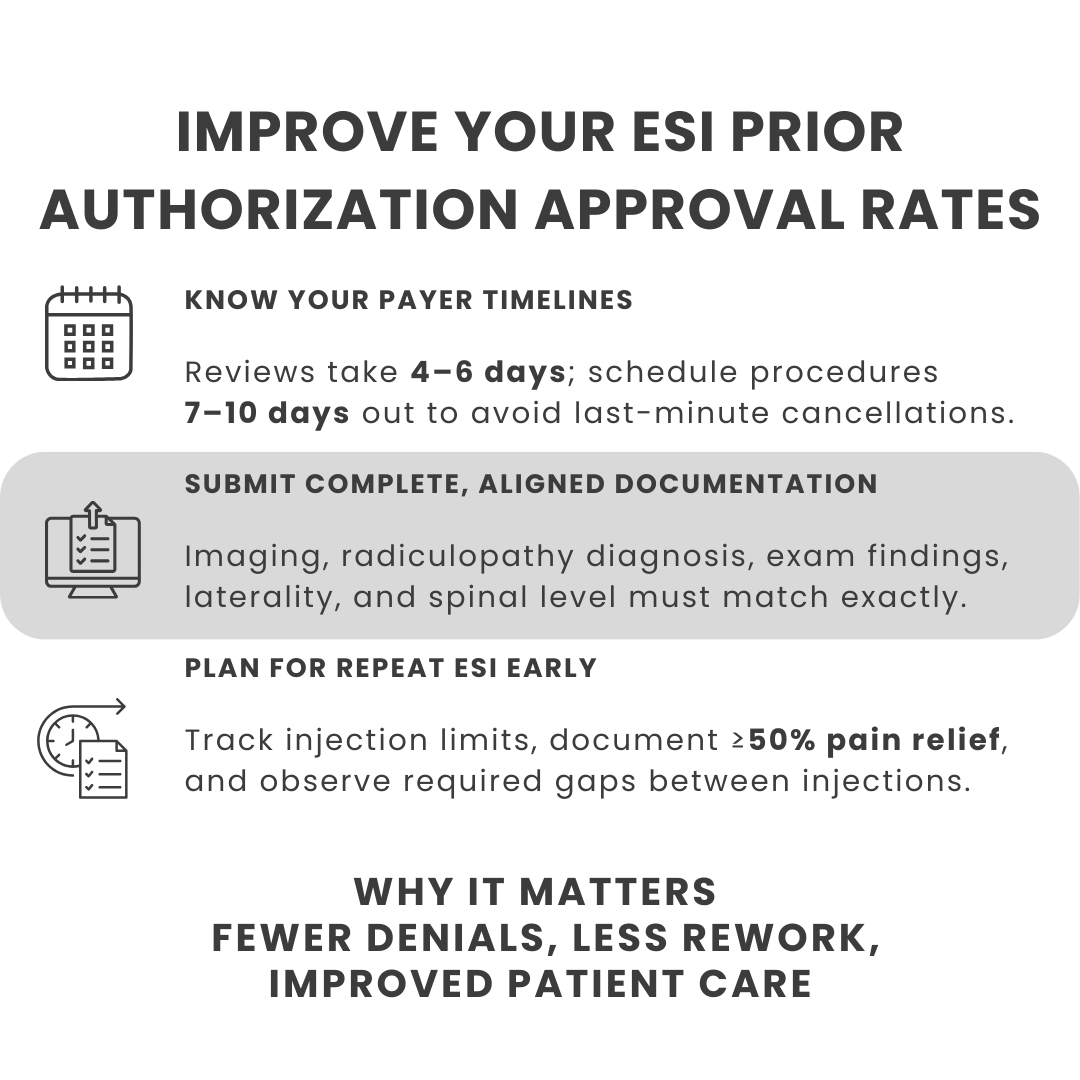
Three High-Impact Tips to Improve SCS Prior Authorization Approval Rates
Below are the three actionable strategies that can immediately improve your SCS prior authorization success and reduce preventable denials:
Step 1: Understand Payer Timelines and Requirements
Most payers take about two weeks to review and approve a prior authorization request. That’s why you should avoid scheduling the patient for at least three weeks after submission. This built-in buffer helps you prevent last-minute cancellations and rescheduling delays, one of the biggest sources of patient frustration.
If you schedule too soon and the authorization isn’t approved in time (which happens often with SCS), the appointment must be pushed out. Patients may have already taken time off work, arranged childcare or transportation, or mentally prepared for the procedure, making the disruption even more stressful.
You should also understand payer policy nuances. For example, United Healthcare frequently routes SCS submissions to peer-to-peer review, which adds more time to the process. Being prepared for these extra steps ensures smoother scheduling and fewer unexpected delays.
Step 2: Ensure Every Required Document Is Complete and Accurate
To avoid unnecessary denials, you must have all required documentation in place before submitting an SCS prior authorization request. This includes:
- Imaging that corresponds directly to the patient’s pain
- A detailed record of conservative therapies tried, along with their outcomes
- Documentation of functional limitations
- A pain diagram and full pain history
- A psychological evaluation
- And most importantly, a provider attestation clearly explaining why the patient is a suitable candidate for neuromodulation
Having each of these elements documented cleanly and consistently helps support medical necessity and significantly reduces back-and-forth with payers.
This may be the most important step. Successful SCS prior authorization isn’t just the responsibility of providers. It depends on full participation from every stakeholder, including the front desk team, medical assistants, and anyone else involved in scheduling, documentation, or follow-up.
Step 3: Involve Every Stakeholder in the Workflow
This may be the most important step. Successful SCS prior authorization isn’t just the responsibility of providers. It depends on full participation from every stakeholder, including the front desk team, medical assistants, and anyone else involved in scheduling, documentation, or follow-up.
When the entire team understands the process, timelines, and documentation requirements, your practice becomes far more efficient. Implementing this coordinated approach not only improves prior authorization approval rates but also increases the likelihood of clean claims getting paid downstream.
Improve your team’s accuracy and streamline SCS submissions with our one-page, clinic-ready checklist
| 👉 Improve your team’s accuracy and streamline SCS submissions with our comprehensive clinic-ready checklist. ⬇️Download the SCS Prior Authorization Submission Checklist |
Why Optimizing SCS Prior Authorization Matters
Poorly managed SCS workflows result in:
- Treatment delays for patients who are already in chronic pain
- Significant administrative strain on clinical and billing teams
- Greater risk of denials, rework, and disruptions to practice revenue
SCS is a high-value, high-scrutiny procedure — and tightening your prior authorization process is one of the most effective ways to minimize risk.
| 📹Watch the Video Here |
The SCS prior authorization process isn’t simple, and its many payer-specific nuances require a careful, informed approach.
The tips shared in this episode are meant to help your team build that foundation.
As this educational series continues, we’ll keep exploring practical, real-world strategies that help practices stay ahead of evolving requirements, minimize denials, and strengthen operational performance.