The healthcare landscape is constantly evolving, with insurance companies setting stringent criteria for reimbursement based on “medical necessity.”
This often presents significant challenges for practitioners, particularly those operating clinics near state lines.
In this blog, we’ll explore the concept of medical necessity, the impact of varying state guidelines, and how these differences create operational and financial hurdles for healthcare providers.
What is “Sufficient Conservative Therapy?”
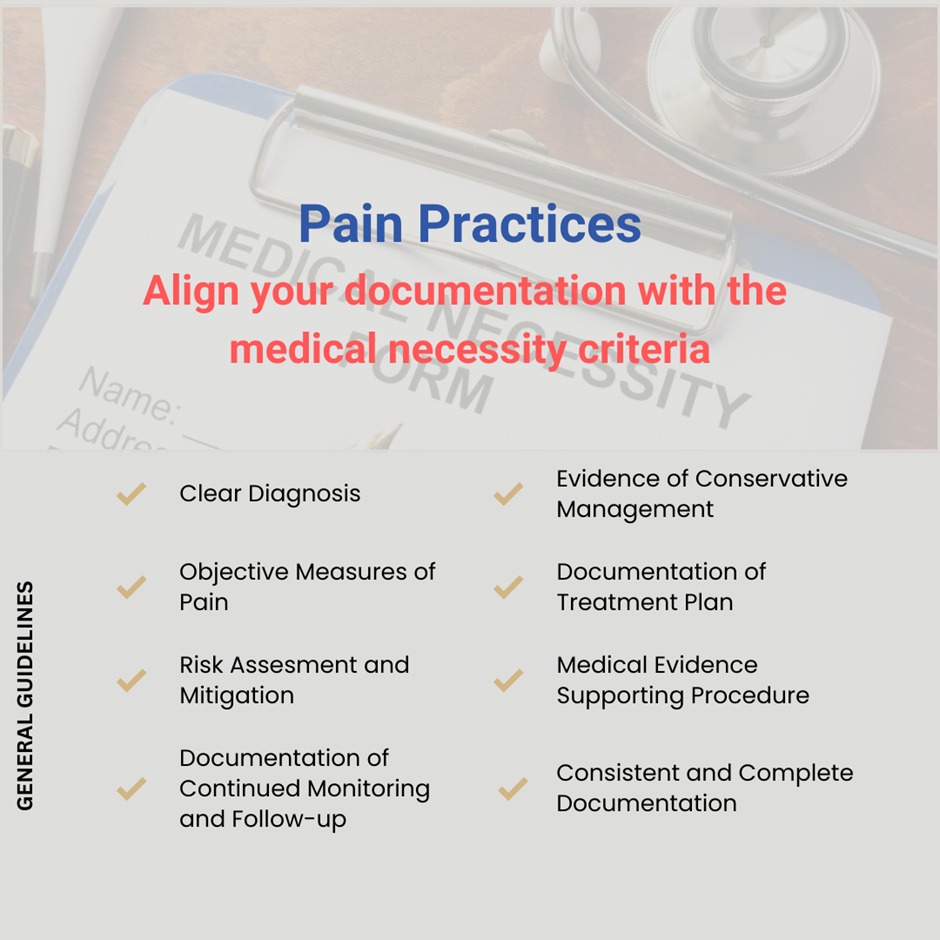
Medical necessity is a framework used by insurance companies to assess whether a procedure or treatment is essential for a patient’s condition. These evaluations are often guided by clinical guidelines devised by insurers’ own physicians and clinicians.
That said, the interpretation of medical necessity can vary significantly, creating challenges for providers. For example, insurers increasingly require practitioners to exhaust conservative therapy options—such as physical therapy or home exercise regimens—before approving more invasive procedures.
However, what qualifies as sufficient conservative therapy often varies by location, even between neighboring states.
Complications for Clinics Near State Lines
1. Variability in Medical Necessity Guidelines
Consider the scenario of a pain management doctor with clinics in North Carolina and South Carolina. It is common for such practitioners to split their time between locations, supplementing care with nurse practitioners and other clinicians.
Medical necessity guidelines can vary significantly between states, even for the same condition:
🔹 North Carolina: Requires three weeks of physical therapy before an invasive procedure.South Carolina: Mandates three months of physical therapy for the same treatment.
This discrepancy creates confusion for providers and patients alike. A doctor cannot feasibly adjust their practice style to accommodate different guidelines across two locations just 10 miles apart. Moreover, practitioners may be unaware of these subtle yet critical differences, leading to compliance risks and potential claim denials.
This variation also affects prior authorization processes, as insurers may require pre-approval for certain procedures based on whether conservative therapy guidelines have been met. A lack of alignment with state-specific requirements can result in delays or denials, even before claims are processed.
2. Reimbursement Rate Disparities
Another major issue is the significant difference in reimbursement rates between states. Using the same example:
- North Carolina might offer higher reimbursement rates than South Carolina for identical procedures.
- If a provider submits claims incorrectly due to system misconfiguration, they may inadvertently accept lower reimbursement rates from South Carolina insurers.
The underlying issue often lies in EMR system configurations that fail to account for state-specific requirements.
Many clinics use a unified system for cost efficiency and consistency. However, when claims are submitted to the wrong state or payer, the lower reimbursement rates apply, and practices face delays in identifying and rectifying these discrepancies.
Operational and Financial Implications
Operating clinics near state lines introduces several operational and financial complexities that extend beyond reimbursement disparities and medical necessity variations. Addressing these challenges is essential for maintaining compliance and financial stability.
- System Configuration Challenges
Practices must ensure their billing systems are configured to submit claims to the appropriate state and payer.
A unified system might simplify operations, but if it cannot differentiate between state-specific requirements, it can lead to revenue losses. Incorrect claim submissions often trigger a cascade of issues, including delayed payments, underpayments, and even audits.
- Complexity of Medicare Guidelines
In addition to private insurers, Medicare poses unique challenges. Different Medicare administrative contractors (MACs) manage regions near state lines, often with unique guidelines and conservative therapy requirements.
Navigating these differences requires meticulous attention to detail and a robust understanding of each agency’s policies.
- Staff Training and Turnover
Another often overlooked challenge is the need for adequately trained staff who can handle the nuances of state-specific regulations and payer requirements.
In border clinics, the administrative burden increases significantly as staff must process claims, verify benefits, and follow up with payers in multiple states.
High turnover rates—a common issue in healthcare—can exacerbate these problems, leading to operational inefficiencies and increased denial rates.
- Patient Communication Gaps
Variations in medical necessity guidelines and conservative therapy requirements can also confuse patients, particularly those who visit clinics in different states.
Patients might not understand why the same procedure is approved in one clinic but delayed or denied in another. This can lead to dissatisfaction, reduced trust in the practice, and potentially a loss of repeat business.
Effective communication strategies are critical to managing patient expectations and ensuring adherence to treatment plans.
Partner with PainMed-PA to Navigate Multi-State Challenges
At PainMed PA, we offer tailored solutions to help your practice thrive near state lines. From comprehensive medical billing to advanced prior authorization management and cutting-edge AI-powered tools, we simplify the intricacies of managing multi-state operations.
Here’s how our services align with the unique needs of multi-state operations:
- Pre-Visit Optimization:
Ensure compliance with medical necessity and conservative therapy requirements through accurate eligibility verification, financial counseling, and prior authorization assessments, reducing delays and denials.
- Post-Visit Precision:
Address reimbursement challenges with meticulous claim scrubbing, denial analysis, and chart reviews, ensuring compliance and recovering lost revenue efficiently.
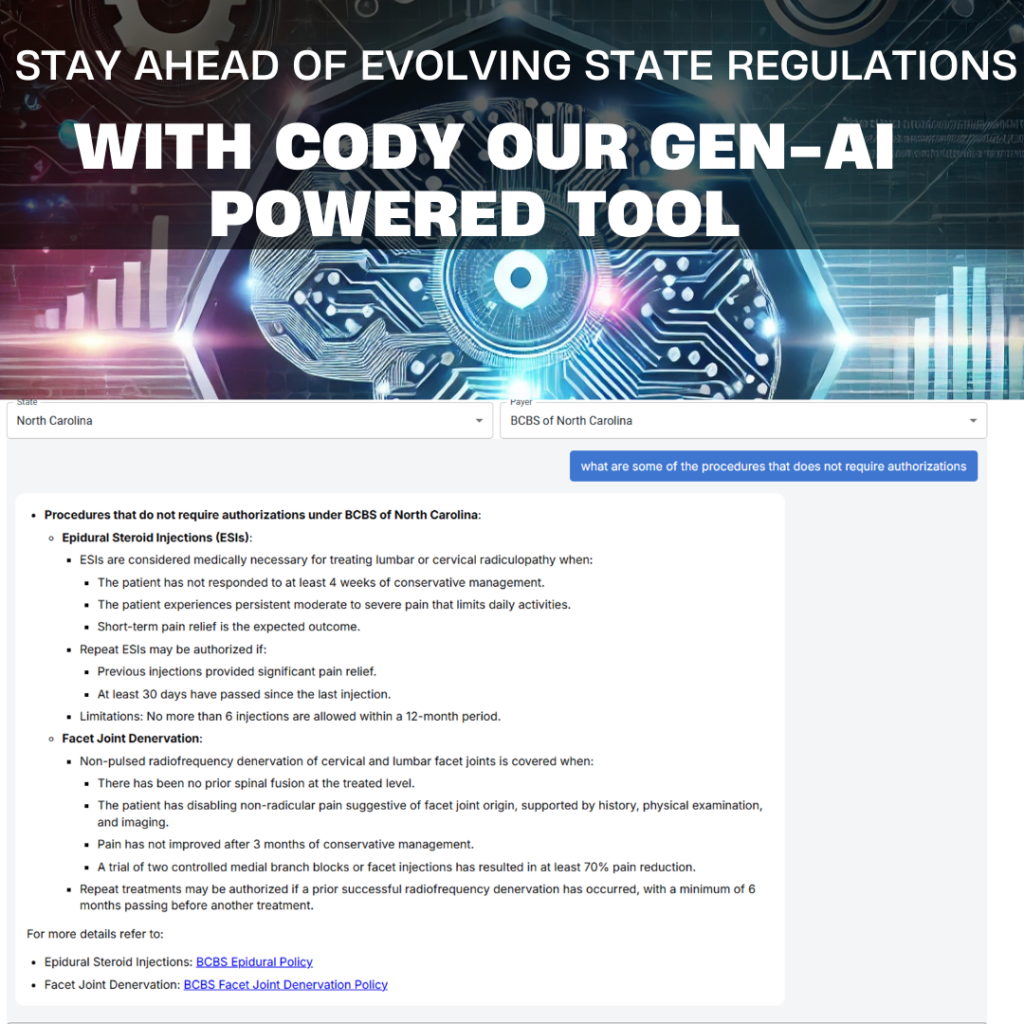
- GenAI-Powered Compliance Tools:
Cody, our proprietary GenAI-powered solution, keeps your clinic updated on the latest payer and conservative therapy guidelines.
It provides real-time compliance checks, automates guideline tracking, and reduces administrative workload, enabling you to stay ahead of evolving state regulations.
- EMR-Agnostic AR Tracking Tool:
Streamline claims processing with our AR tracking tool, which integrates with any EMR system to analyze claims data, identify patterns, and prevent reimbursement delays.
Our results speak for themselves: a 95% net collection ratio with days in AR less than 21 days.
Are You Ready to Simplify Multi-State Operations? Call us at (512) 868 1762.