Kyphoplasty is among the most heavily audited procedures in interventional pain and spine practices. Across multiple payers, practices are experiencing high prior-authorization denial rates, as well as claim denials even after authorization has been granted.
In most cases, these denials are not driven by the technical performance of the procedure, but by coding errors, incomplete documentation, insufficient imaging correlation, or gaps in medical-necessity support.
| Medical & Coding Information Disclaimer This content is provided for informational and educational purposes only and does not constitute medical advice, clinical guidance, or billing recommendations. Coverage, coding, and documentation requirements vary by payer and patient-specific factors. Providers should consult applicable payer policies, clinical judgment, and official coding resources before making treatment or billing decisions. |
As payer review intensifies, this article brings together the key clinical, coding, and documentation requirements for CPT® 22514 to help providers support medical necessity and reduce avoidable denials.
What is Kyphoplasty and how does CPT® 22514 affect coverage and audit risk?
Kyphoplasty is a form of percutaneous vertebral augmentation (PVA) used to stabilize painful vertebral compression fractures (VCFs) and improve functional outcomes in carefully selected patients. In interventional pain and spine practices, kyphoplasty is most commonly performed for fractures related to osteoporosis, malignancy, or selected traumatic mechanisms that do not require open surgical intervention.
From a coding standpoint, CPT® 22514 represents kyphoplasty performed at the first treated lumbar vertebral body during a session. This code is subject to significant payer scrutiny, making comprehensive clinical documentation, imaging correlation, and adherence to payer medical policies essential for coverage, reimbursement, and audit defense.
What is the clinical purpose of Kyphoplasty in Lumbar Vertebral compression fractures?
Percutaneous vertebral augmentation of a lumbar vertebra is performed to:
Stabilize a painful vertebral compression fracture
- Reduce mechanical pain
- Improve functional mobility
- Prevent progressive vertebral body collapse
- Avoid open spinal surgery in appropriately selected patients
Kyphoplasty is typically indicated when pain persists despite conservative therapy or when the underlying pathology (such as malignancy) warrants earlier intervention. The procedure is not intended as a first-line treatment for nonspecific low back pain.
Which patients are appropriate candidates for Kyphoplasty?
Appropriate patient selection is fundamental to both clinical outcomes and medical-necessity determinations.
Clinical Selection Criteria
Symptomatic lumbar vertebral compression fracture
- Focal back pain that correlates with imaging findings
- Pain persists despite adequate conservative management, unless:
- Fracture is malignant
- Severe functional impairment justifies earlier intervention
Common Etiologies
- Osteoporosis
- Osteolytic metastases
- Multiple myeloma
- Select traumatic fractures without burst morphology
Contraindications
- Spinal canal compromise requiring decompression
- Neurologic deficit attributable to retropulsed fragments
- Active systemic or local infection (e.g., osteomyelitis, epidural abscess)
What imaging is required to establish Medical necessity?
Imaging confirmation is a core requirement across payer medical policies.
Preferred Imaging
- MRI of the lumbar spine
- Confirms fracture acuity via marrow edema
- Correlates pain with fracture level
Alternative / Adjunct Imaging
- CT
- Evaluates posterior wall integrity
- Excludes burst fracture morphology
Key Imaging Elements That Should Be Documented
- Vertebral level(s) (e.g., L2, L3)
- Vertebral height loss and configuration
- Evidence of acute or subacute fracture
- Absence of canal compromise or infection
How does CPT® 22514 define the procedure?
CPT® 22514 describes:
Percutaneous vertebral augmentation, including cavity creation using balloon or mechanical device, unilateral or bilateral cannulation, including all imaging guidance; lumbar.
Key coding principles:
- Reported once per lumbar vertebral body
- Applies to the first treated lumbar level
- Imaging guidance is bundled and not separately reportable
- Unilateral vs bilateral access does not affect units billed
Authoritative reference:
https://www.aapc.com/codes/cpt-codes/22514
Which CPT® codes are used for Vertebral Augmentation by region?
Vertebral Augmentation CPT® Code Family
| Service Focus | Primary Code (First Level) | Add-On Code (Each Additional Level) |
| Thoracic vertebra | 22513 | 22515 |
| Lumbar / Sacral vertebra | 22514 | 22515 |
Which ICD-10-CM Diagnosis codes commonly support CPT® 22514?
Common ICD-10-CM Pairings
| Clinical Condition | ICD-10-CM Code |
| Osteoporotic vertebral compression fracture | M80.0xxA |
| Pathologic fracture due to neoplasm | M84.5xxA |
| Multiple myeloma with bone involvement | C90.00 |
| Secondary malignant neoplasm of bone | C79.51 |
Diagnosis coding should:
- Reflect fracture etiology
- Capture acuity and encounter type
- Avoid unspecified fracture codes when possible
What documentation is required to support CPT® 22514?
Documentation Essentials
- Clinical diagnosis with fracture etiology
- Imaging confirmation (MRI or CT)
- Conservative therapy attempted (unless malignancy/severe impairment)
- Pain severity and functional limitation
- Vertebral level(s) treated
- Procedure plan and technique
- Risk discussion and informed consent
Operative Report Should Include
- Access route
- Cavity creation method
- Cement type and volume
- Intra- and post-procedure neurologic status
- Complications (if any)
| Need Support With Kyphoplasty Documentation or Prior Authorization? Is your practice facing repeated denials, documentation gaps, or payer questions for CPT® 22514? Our team supports interventional pain practices with documentation review, prior-authorization readiness, and audit-focused workflows for kyphoplasty. 📩 Contact our team for kyphoplasty documentation support. |

Why is Kyphoplasty closely reviewed under WISeR programs?
Under Wasteful and Inappropriate Service Reduction (WISeR) initiatives, vertebral augmentation procedures are frequently reviewed for:
- Clear pain–imaging correlation
- Appropriateness of conservative management
- Use of augmentation as part of a structured care plan
Strong, consistent documentation by the provider is the primary safeguard against denials and post-payment audits.
What are the common coding and audit risks for CPT® 22514?
- Incorrect regional code selection (22513 vs 22514)
- Billing imaging guidance separately
- Reporting per pedicle rather than per vertebral body
- Missing conservative-therapy documentation
- Poor alignment between imaging and symptoms
Frequently Asked Questions
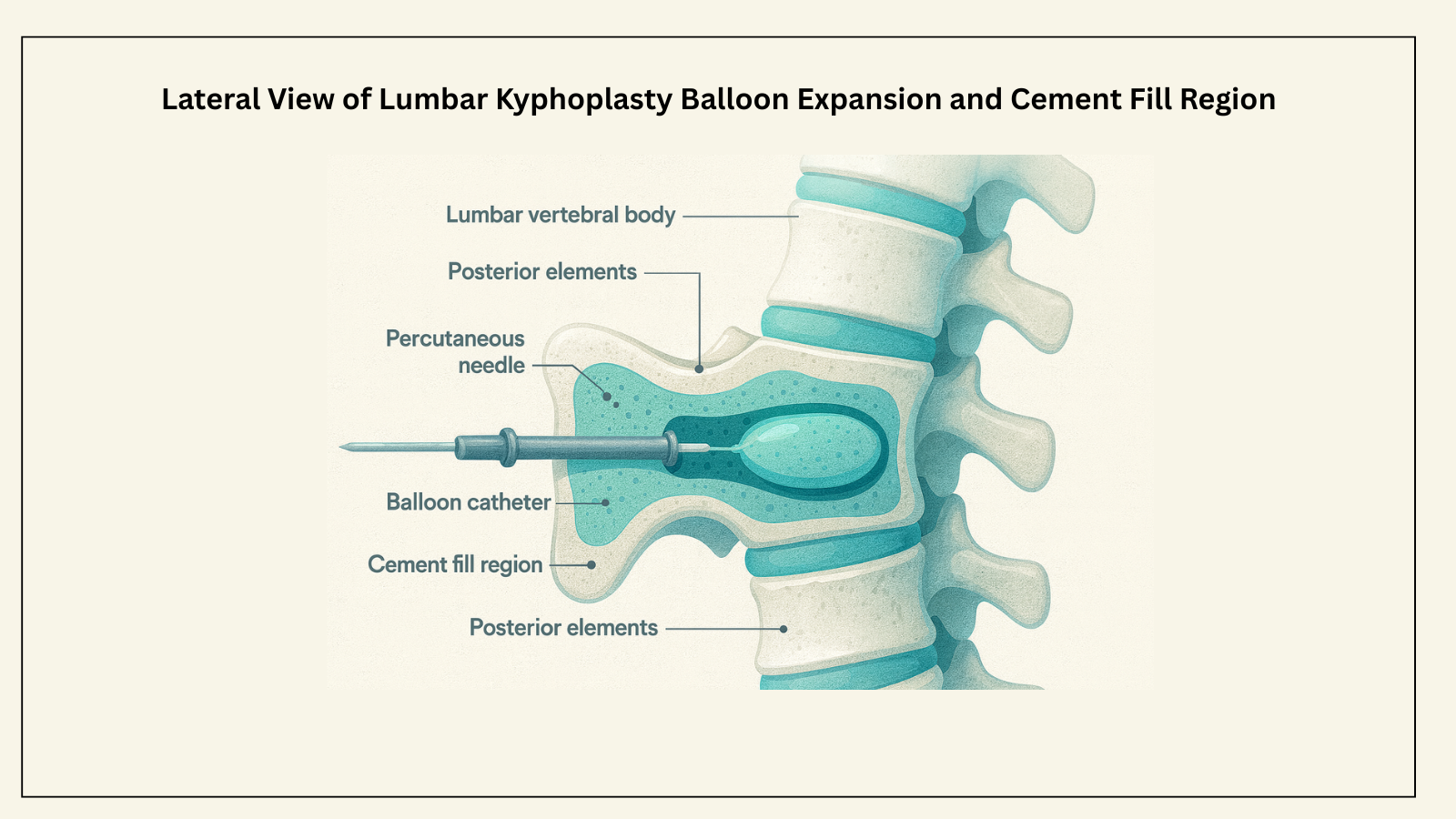
- What Anatomical Structures Are Relevant to Kyphoplasty of the Lumbar Spine?
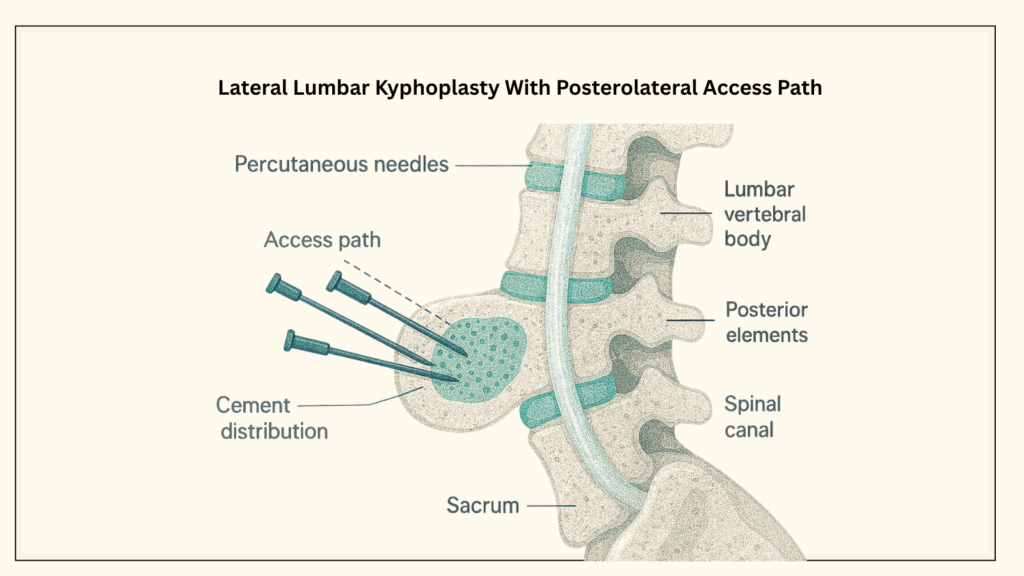
The lumbar vertebral body is a cylindrical, anterior load-bearing structure composed primarily of cancellous trabecular bone surrounded by a cortical shell. The superior and inferior endplates interface with the intervertebral discs.
Posteriorly, the vertebral arch—including the pedicles, laminae, and spinous process—protects the spinal canal and neural elements. During percutaneous augmentation, the provider targets the cancellous portion of the fractured vertebral body while avoiding:
- The posterior vertebral wall
- The spinal canal Neural foramina
- Epidural venous plexus
Access is typically achieved through a transpedicular or parapedicular/posterolateral approach under continuous fluoroscopic or CT guidance.
- How Is Kyphoplasty Performed Step-by-Step?
Kyphoplasty is performed under continuous imaging guidance and typically includes:
- Patient positioning (prone) with local, monitored, or general anesthesia
- Percutaneous cannula placement via transpedicular or parapedicular access
- Balloon inflation or mechanical cavity creation
- Low-viscosity PMMA cement preparation
- Controlled cement injection while monitoring for leakage
- Instrument removal and sterile dressing placement
Many patients are able to ambulate the same day and experience rapid pain relief when appropriately selected.
- How Should Additional Levels Be Reported During the Same Session?
- Report CPT® 22514 for the first lumbar vertebra treated
- Report CPT® 22515 for each additional thoracic, lumbar, or sacral vertebral body treated during the same operative session
The unit of service is per vertebral body, not per pedicle or per side.
- Is Imaging Guidance Separately Billable With CPT® 22514?
No. Fluoroscopy or CT used for kyphoplasty is bundled into CPT® 22514.
- Does Bilateral Access Allow Multiple Units of CPT® 22514?
No. CPT® 22514 is reported once per vertebral body.
- Can a Bone Biopsy Be Performed During Kyphoplasty?
Yes, if medically indicated, but it does not change CPT® selection and must be clearly documented.
- Is Prior Authorization Usually Required?
Yes. Most payers require imaging, conservative-therapy documentation, and medical-necessity justification.
Kyphoplasty under CPT® 22514 is a high-scrutiny procedure where coverage decisions depend heavily on documentation quality, imaging support, and adherence to payer medical policies.
Clear patient selection, well-documented conservative management when appropriate, precise procedural notes, and accurate coding are essential to support medical necessity. Practices that consistently align these elements are better positioned to reduce denials, withstand audits, and ensure compliant use of vertebral augmentation.
Author:
Rajanikanth Kanyaboina, CEO and Co-founder: PainMed-PA
Rajanikanth Kanyaboina has over 18 years of impactful experience shaping strategy and commercial outcomes in healthcare. With a strong background in healthcare reform, population health, and Health-IT interoperability, Raj specializes in identifying new markets, scaling innovations, and enabling collaboration across payors, providers, pharma, and technology vendors. Raj has held progressive leadership roles spanning strategy, business development, P&L management, and partner ecosystems.
| Do your kyphoplasty notes clearly support medical necessity before prior authorization or review? Download the Kyphoplasty (CPT® 22514) Clinical & Coding Playbook A structured, payer-aligned reference covering patient selection, imaging requirements, CPT® & ICD-10-CM pairing, documentation essentials, and common audit risks. ⬇️ Download the Playbook |