In our earlier article, “What Should Independent Practitioners Know About Medicare’s Prior Authorization Pilot Beginning in January 2026?”, we outlined the scope, structure, and operational implications of CMS’s new WISeR (Wasteful and Inappropriate Services Reduction) Model under Traditional Medicare.
Building on that foundation and informed by the discussion captured in the video embedded below, this article examines the broader implications of WISeR for interventional pain practices.
That article focused on what is changing.
This one asks a harder question:
What does WISeR actually mean for interventional pain practices in the real world, and who bears the risk if the model scales nationally?
Early signals from across the interventional pain management landscape suggest that WISeR is not just a six-state pilot. It may represent the beginning of a tech-first utilisation management era, one that fundamentally changes how providers are evaluated, reimbursed, and ranked.
WISeR is likely to expand beyond the pilot
Although CMS has framed WISeR as a limited pilot involving 17 services across six states, there are strong indications that this scope is unlikely to remain static.
“We don’t believe this will stop at just six states and 17 procedures. Adoption is likely to expand rapidly.”
Historically, CMS pilots that demonstrate cost containment, especially those involving utilization controls, have tended to scale nationally or influence commercial and Medicare Advantage payer behavior.
For independent pain practices, this means WISeR should be treated not as a temporary compliance hurdle, but as a signal of what’s coming next.
The 90% approval target: a quiet but powerful shift
One of the least discussed but most consequential elements of WISeR is the 90% approval (affirmation) benchmark tied to potential “gold status.”
Practices that consistently meet this threshold may qualify for reduced prior authorization requirements in the future.
On paper, this sounds like relief.
In reality, it introduces a fundamental shift:
Practices are no longer evaluated primarily on clinical outcomes but on their ability to submit flawless prior authorization documentation.
This creates several downstream effects:
- Approval rates become a performance metric
- Documentation quality outweighs clinical nuance
- Administrative precision directly impacts future workload
| Want to Understand What WISeR Means for Your Practice? If you’re evaluating how the WISeR Model could impact your workflows, approval rates, or revenue cycle and what steps to take next, call us at (512 ) 868 1762 |
For practices without dedicated PA teams, this creates a high-stakes documentation environment where small errors compound into systemic disadvantage.
A tech-first review model changes the rules of the game
WISeR is ushering in a tech-first adjudication model, where:
- Prior authorization requests and claims are first screened by algorithms
- AI determines whether a request advances to clinical review or is denied outright
- Human review happens after technology-based triage
This matters because AI-driven screening does not interpret nuance the way clinicians do.
Under this model:
- Claims with modifier 25 may be denied automatically
- Previously tolerated coding variations may now trigger instant rejection
- Documentation gaps that once led to follow-up requests may now result in denials
In short, technology becomes the gatekeeper, not the clinician.
WISeR risks penalizing smaller, independent practices Large health systems and management groups already operate with:
- Centralised PA teams
- Advanced revenue cycle software
- AI-assisted coding and compliance tools
Independent practices, by contrast, often rely on:
- One or two multirole staff members
- Manual documentation workflows
- Provider-driven chart completion
Under WISeR, this imbalance becomes more pronounced.
If approval rates determine future administrative burden, practices without the infrastructure to optimize PA workflows early may find themselves trapped in permanent high friction mode while larger systems accelerate ahead.
Coding errors become immediate financial threats
Another critical concern is that WISeR dramatically compresses the margin for error.
In the past:
- Coding issues triggered rework, appeals, or clarification
Under a tech-first model:
- Errors trigger automatic denials
- Appeals consume additional time and resources
- Cash flow disruption becomes routine
For high-cost procedures like epidural steroid injections, even a small number of denials can materially impact monthly revenue.
Is WISeR changing how providers are measured and paid?
CMS has positioned WISeR as a safeguard against fraud, waste, and abuse. That objective is not controversial.
What raises concern is how that objective is being operationalized.
WISeR appears to:
- Incentivize documentation behavior over clinical judgment
- Shift administrative risk downstream to providers
- Normalize AI-first decision making across payers
If this model expands as early indicators suggest may redefine what “compliance” means in everyday practice.
Why this critique matters now
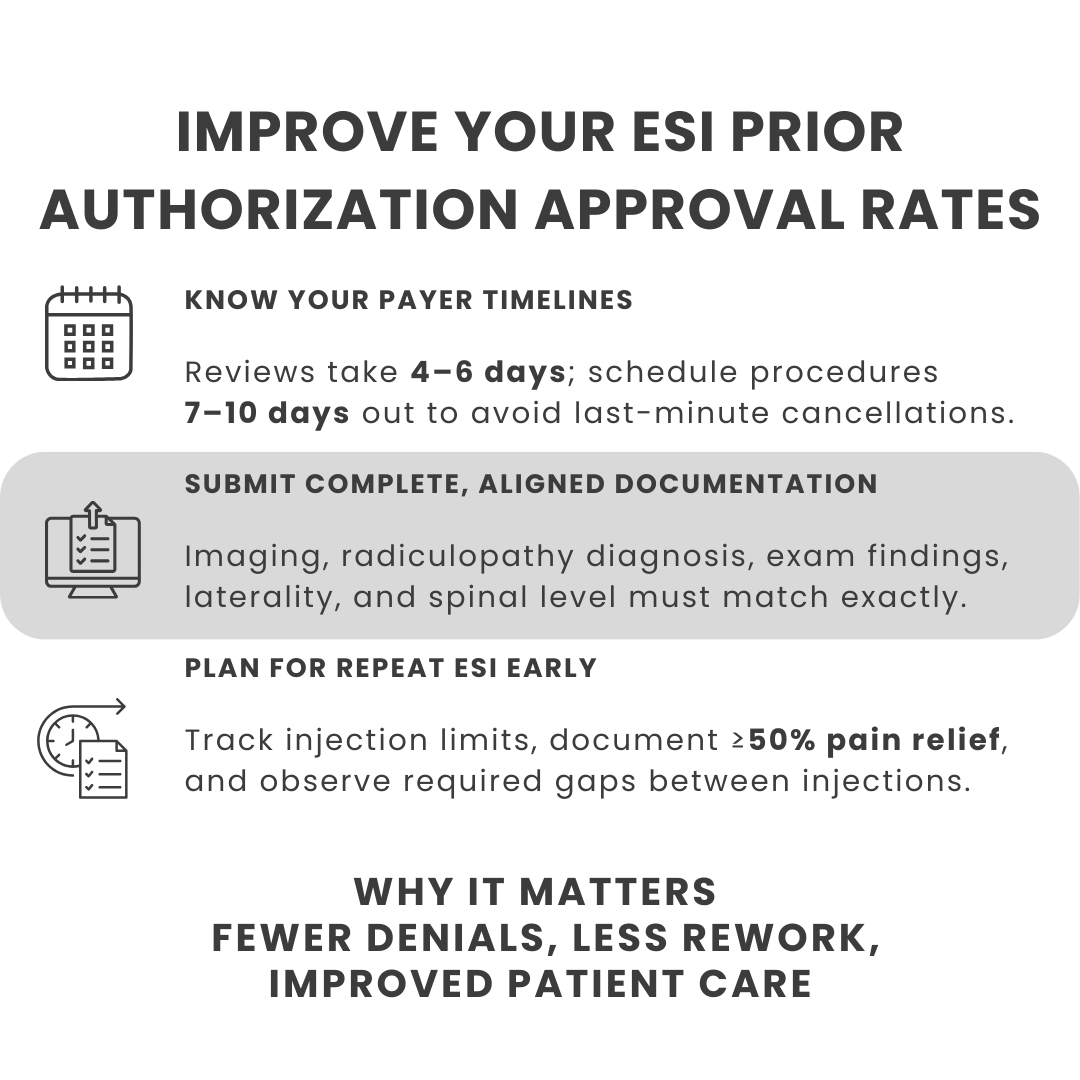
Our earlier article explained how to prepare for WISeR.
This critique explains why preparation is non-negotiable.
WISeR is not simply about submitting more paperwork. It is about:
- Adapting to algorithm driven utilization management
- Protecting approval rates as a strategic asset
- Reengineering workflows before denials become normalized
For independent pain practices, early adaptation may be the difference between earning future exemptions and operating under perpetual administrative strain.
The real risk of WISeR is complacency
WISeR does not eliminate clinical autonomy overnight.
But it quietly redefines the rules of reimbursement.
Practices that wait until denials increase, payments slow, or approval rates fall may find themselves reacting too late.
| Watch the video here |
As this model spreads, the practices that endure will be the ones that treat prior authorization not as clerical work but as a strategic function.
Presented by:
Rajanikant Kanyaboina, CEO and Co-founder: PainMed-PA
Rajanikanth Kanyaboina has built his career entirely in healthcare, spanning over 20 years and gaining formative experience at large healthcare and health IT organisations, which has provided him with a practical understanding of the industry across payers, providers, and pharmaceutical companies.
His perspective shifted after co-founding an independent pediatric practice, where he experienced firsthand the operational realities of running an independent, physician-owned practice.
That experience led to the creation of Probe Practice Solutions and Painmed-PA, using technology to reduce administrative burden and support independent practices.
His work focuses on helping independent practices operate efficiently while staying centered on patient care.
Kalyan Yamijala, COO and Cofounder: PainMed-PA
Kalyan Yamijala has spent over 25 years at the intersection of healthcare and technology. As a founder of a healthcare technology and revenue cycle management company, he’s passionate about creating smart solutions that make medical billing simpler, streamline revenue processes, and ultimately improve patient care.